Role of Physical Examination in 21st Century
Role of Physical Examination in 21st
Century
What If the Revolution Lies Within our Reach?
Yanis AFIR
Physical examination has always played a very important role in medical practice. However, it has lost a consequent amount of its value to new technologies and diagnostic methods. In this short review, we will discuss some of the issues faced by classic bedside physical examination in order to keep up with the challenges of the 21st century.
Even though
the topic of this issue is The History of Medicine, we might have, confidently,
written this article in the previous one. Indeed, in this era where technology
dominates and primary care has nearly lost its humanistic dimension, the classical
physical examination and the dogma it represents plays a very important role in
keeping the balance in medicine and might truly be the next “Cutting-Edge” of
medical practice. A real revolution might very well come from our stethoscopes
and reflex hammers...
Bedside
physical examination has been a part of medicine from the beginning. Actually,
for a very long time, its first pillar, the observation (or inspection),
represented almost the whole of medical practice. However, physical
examination really took a step forward and became truly scientific or
“clinical” starting only from 18th century. Two main events mark this period.
First, in Austria, Joseph Leopold von Auenbrugger observed his father, an
innkeeper, tapping on barrels and, from the produced sound, establishing
whether wine has yet reached the proper quality. Auenbrugger tried to use the
same technique to detect abnormalities in the chest and described it in his
book “Inventum Novum”. This is how Percussion was born and added to
physical examination.
Few years
later, in Paris, René Lænnec, finding it somewhat inappropriate to stick his
head in young ladies’ chests in order to listen to their hearts, had the idea
of a little cylinder which he used to listen to heart abnormalities from a
safe distance. After describing this tool in his book “De L’auscultation
Mediate, Traité du Diagnostic des Maladies des Poumons et du Coeur,” people
developed it, and later it led to the stethoscope.
The
invention and development of these new techniques brought a real revolution in
medicine; in fact, we can state that modern medicine was invented in that era,
as it was only then that healers really started making diagnoses.
However, we
can easily notice a net drop in the classical bedside medicine in favor of new
technologies. Technologies, of course, are necessary and have led to many
breakthroughs in medical research; however, considering the primary healthcare
and the way we deal with patients, it is sad to realize how we moved from a
philosophy of medicine in which the patient is in the center of the inquiry to
an environment full of computer devices and TV screens, where most of the
discussions (and studies) occur away from the patient.
 |
| Luke Fildes – The Doctor. 1891. Source |
The image above is a famous painting by Luke Fildes named “The Doctor”. We are not quite qualified to play the art critic, but something is really interesting about the painting : Fildes has perfectly captured the medical spirit of his era. A Doctor, sitting in a chair and looking at a sick little child. There is no physical barrier between them (indicating probably that there is no psychological barrier either). There is no book, no instrument and no complicated data or sophisticated machine; his eyes stare at the little child, not disturbed by the cup of tea that he had been given, nor the mother’s tears. The father seems to not even dare talk to him. The Doctor seems to have interrupted all the circuits of his brain to focus on one task only, saving this little girl... Alright, we may have exaggerated a little bit, but you get the point!
What if all
the doctors had been like this one? What if we treated our patients like our
own lives were at stake?
Let’s go
back to reality now. You have a very bad abdominal pain and you decide to go to
the hospital. Without any overstatements, the image below is very close to what
actually happens in our emergency rooms. Instead of focusing on the patient’s
needs and trying to understand his complaint, we rather launch series of
expensive, useless and sometimes dangerous, tests where a simple patient
history and proper physical examination would have been more than enough.
We can not
in our modest review enumerate all the causes that pushed us away from our
patients, nor can we nominate solutions. Thus, we will simply try to highlight
the major challenges for physical examination.
The first
issue is the lack of research and the necessity and benefit of promoting it in
classic bedside examination. The second point is about rationalizing the
physical examination and applying the researches results in an Evidence-based
approach. Finally, we will try to discuss the challenges of physical
examination’s assessment in medical school.
A lack
in research
There are
many books dedicated to physical examination, with usually high-quality
explanations and illustrations. From medical school textbooks to whole signs
dictionaries, one can easily find a great reference to study from.
Nevertheless, we are forced to state that the scientific value of the
information and the quality of evidence is in many cases very poor. We mean
that, apart from general principles agreed on, many of the presented
statements, observations, rules and even tricks often result from the author’s
own experience, far from a strong evidence and with complete disregard to
research findings and latest data.
The reason
behind this is beyond the authors of these textbooks and lies in research
itself. Very few researches are conducted to study the bedside examination compared
with other diagnostic tools. Infact, physical examination is only approached in
its pedagogical dimension. It is considered more of an “art” than a real
science. Perhaps this is the reason that pushed some prestigious authors to
name their books “Art & Science”1, 2, as to remind us that there is also a
little science in it...
We look at
physical examination only as a mandatory step in medical curriculum, taught
only out of habit or tradition. Take a student who is having his first physical
examination lecture; the joy and happiness of finally acting like a real
doctor is very quickly replaced by the disappointment of noticing that none of
his teachers really apply what they are teaching in their daily practices, not
even a half of it! If that wasn’t enough, these same “teachers” pretend to have
the ability to evaluate students... have you felt that frustration too?
Sorry... let’s go back to research.
As said
earlier, the number of papers talking about physical examination is really
small. We can mention three great initiatives that promote Evidence-based
physical examination: “The Rational Clinical Examination” systematic reviews
series in JAMA (Journal of The American Medical Association)3; the book “Evidence-Based
Physical Diagnosis” written by Steve McGee4 and the Stanford25 education
initiative5.
As a matter
of fact, in 15 years, only about 70 articles were published in The Rational
Clinical Examination. If you don’t see how little this is, maybe it will help
you to know that approximately 2000 new articles are indexed in PubMed every
day6!
The reason
behind this lack in meta-analyses and systematic reviews is that the number of
data available is very poor. Most of the studies include far less than 100
patients, sometimes only 2, and are old and conducted in questionable
conditions. Even worse, we can evaluate the quality of evidence only after
having done all the standardization and analysis, to often discover that the
data is useless, discouraging researchers even more.
The
initiators of the Rational Clinical Examination wanted to “restore
respectability to a part of medicine that seemed to have been eroding as academic
and financial rewards went to those who most resembled scientists relying on
expensive diagnostic tests and least behaved as physicians relating to patients”,
said Drummond Rennie in his preface3. According to Sackett, there are 5 main
reasons behind the lack of research in physical examination field7:
1- Designing investigations on the
precision and accuracy of the medical history and physical examination is
very arduous. First, we have to assemble a large number of appropriate
patients, then proceed to their repeated examination by clinicians, either
wide-rangingly experienced ones or those still in training, and then proceed
to a gold standard examination, which can vary from the simple imaging to
surgery or autopsy! If the results were inconclusive, the data analysis is
often unorthodox and challenging.
2- A clinical diagnosis rarely resides
in a single symptom or sign, but rather in the patterns emerging from many
symptoms and signs combined. The data is thus subject to multivariate
phenomena.
3- Clinical examination researches
often don’t grant any fame, prestige or reward. In result, researchers
influenced by the exciting challenges and academic rewards, are much more
interested in investigating laboratory or imaging tests.
4- Financial issues are probably the
biggest reason behind this desert in research. Pharmaceutical and medical
technology companies often promote and reward clinicians investigating in
advanced technology. And one must not forget about political and financial purposes
behind this: it is far more interesting for companies to have physicians
buying their “superadvanced” devices than taking their time with a thorough
history taking and physical examination.
5- Finally, as mentioned earlier, many
clinicians still consider bedside diagnosis as an “art” more than a real
science.
At this
point, only one question remains: why is it worth it to invest in physical
examination research? A part of the answer is that these researches could help
make the physical examination so accurate that in many cases we would not need
imaging or laboratory results at all. As an example, Crombie found out that
more than ¾ of the diagnoses in primary care are established after a brief
history and a routine clinical examination8.
Steve McGee
emphasizes on the importance of “Stop rules” in daily practice. These rules
result from combinations of bedside findings that argue so much against the
diagnosis that the investigation should stop and no imaging or laboratory test
is needed9. Examples of these include the Ottawa rules for ankle injury and
the Alvarado score for appendicitis. If such stop rules were applied in the US,
an estimated 700 billion dollars a year spent in unnecessary tests and
procedures would have been saved10.
An Evidence-based
approach4,9
As we
mentioned above, one of the main reasons behind the delay which physical
examination suffers from is the inability of physicians to rationalize their
findings and fully benefit from Evidence-based researches. Here we will try to
give examples of how to effectively use physical examination data.
1-
Sensitivity and Specificity, classic but not very useful
We
perfectly know that biostatistics are a very powerful hypersomnic agent for
most medical students, but we ask our beloved readers to forgive us, we have to
dive into some details... it will be worth it (or else refunded).
As a quick
recap, let’s review the definition of sensitivity and specificity.
Sensitivity
is the ability of a test to be positive in patients who have the disease. In
other words, it is the proportion of patients with the disease who have the
physical sign (i.e., have the positive result).
Specificity
is the ability of a test to be negative in patients who don’t have the
disease. In other words, it is the proportion of patients without the disease
in whom the physical sign is absent.
The
calculation is simple, here is an example: let’s imagine a study of 100
patients to evaluate the power of a certain test to detect a disease. The
following column summarizes the findings:
Remember
that Sensitivity is the number of sick patients with a positive test compared
with the total number sick patients. Thus, it is calculated by the following
formula: Sensitivity = TP/(TP + FN). In this example: 22/(22+20) = 52%.
Specificity
is the number non-sick patients with a negative test compared with the total
number of non-sick patients. Thus, it is calculated by the following formula:
Specificity
= TN/(TN + FP). In this example: 55/(55+3) = 95%.
Knowing how
to calculate is good but dealing with the numbers’ meaning is what is most
important. THAT is far more complex than seemingly thought. Consider a real
example : a 40-year-old man with a history of chronic alcohol consumption comes
to your office complaining of an increased abdomen volume. At a first glance,
and given the history of the patient, you think of an ascites. Rather than
directly requesting an abdominal ultrasound, you want to figure out how well
physical examination alone can detect ascites. After a little research, you
find 3 meta-analyses that reported the results of the different studies11-13. The
following table summarizes the results:
Great, now
that you have the results, do you think you can interpret and use them in your
practice? Let’s start with inspection, Bulging flanks and Edema seem to have
very high sensitivities, which is a really good starting point. But how do you
deal with Bulging flanks specificity? The variation among studies is very
considerable, going from 44% to 70%. It is even worse for Flank dullness, going
from 29% (which is very poor) to 69% (which is quite correct). So the first
difficulty is variation in data results and the inability of making sense of
the numbers. A simple way of correcting the problem is taking the average of
the results. Although not very precise, it may be helpful.
However,
the real problem is when trying to combine data. What do you say about a
patient presenting to the ER with bulging flanks, shifting dullness and fluid
wave but none of the other features? Notice that some signs with very high
sensitivity are absent. On the other hand, some signs with very high
specificity are present... It is very confusing and unless there is an
effective method to combine sensitivities and specificities, we are incapable
of making any decision.
2- More
simple and more practical : The likelihood Ratio
A very
simple, effective and, most important, practical index to use with data is the
Likelihood Ratio (LR). It summarizes the information contained in sensitivity
and specificity to tell us how likely a given test result is in people
who have the disease compared to how likely it is in people who do not have the
disease. This method of describing the accuracy of diagnostic information,
once mastered, is much faster and more powerful than the sensitivity and
specificity approach.
The first
concepts that one must understand are the Pre- and Post-test probabilities.
Pre-test probability is the probability of a person to have a disease before
applying any test on him. In most cases, it corresponds to the prevalence of
the disease in the country. For example, if the prevalence of a certain
disease is 16%, any random patient has a probability of 16% to have that
disease.
Post-test
probability is the probability of a patient to have the disease after
considering the results of a diagnostic test. The shift in the probability
before and after applying the test expresses the « strength » of the test; it
tells us how powerful our test is in recognizing the disease.
We should
also remember that some findings, when positive, increase greatly the
probability, but they change it very little when negative. In opposite, other
signs are more useful if they are absent, because the negative finding
decreases considerably the probability, although the positive one changes
probability very little.
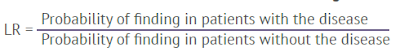
Here, the likelihood ratio is the most useful
tool to show the strength of a test. Its definition is basically « the
proportion of patients with disease who have a particular finding divided by the proportion of
patients without disease who also have the same finding. »4
We add the adjectives « positive » and « negative » to
indicate in which case the physical sign is present or absent. A positive LR,
therefore, is the proportion of patients with the disease who have a physical sign
divided by the proportion of patients without the disease who also have that
sign. A negative LR, is the proportion of patients with the disease who lack a
physical sign divided by the proportion of patients without the disease who
also lack that sign.
The formula is very simple. In a positive LR, the
numerator, i.e « the proportion of patients with the disease who have the
physical sign » is basically the sign’s sensitivity. And the denominator, i.e «
the
proportion of patients without the disease who have the
sign » is the 1- specificity.
Thus: Positive LR = Sensitivity/(1- Specificity).
It seems a bit confusing but try to think of it slowly
and you will see that it is really simple.
Same thing for the Negative LR: the nominator, i.e «
the proportion of patients with the disease lacking the finding », is 1 - sensitivity.
And the denominator, i.e « the proportion of patients without the disease lacking
the finding », is the specificity.
Therefore: Negative LR = (1- Sensitivity)/Specificity.
Now the most most important part: what do these
information tell us ? When the LR of a test is above 1.0, it means that the
finding is more likely among patients with the disease than those who lack the
disease. Thus, a LR > 1 means that the probability of the disease increases.
By applying the same reasoning, we deduce that when the LR is below 1, the
probability of the disease decreases. Finally, when the LR is 1, or very close to
it, it means that the probability of the disease is unchanged
(because the finding is equally likely in patients with
and without the disorder).
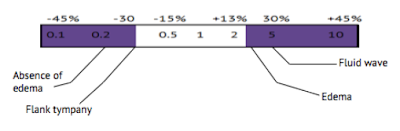
Now let’s apply these findings to our example. Remember
that the Sensitivity of the Edema was 87%, and the Specificity 77%. Thus the
positiveLR = 0.87/ (1- 0.77) = 3.8. The negativeLR = (1- 0.87)/0.77 = 0.2. We
calculate the remaining LRs and summarize the results in the table:
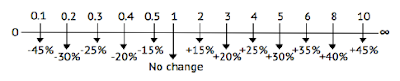
Now that we have all the LRs, the final step is to
know how to use them. With some complicated formulas and statistical methods,
which we will not demonstrate here, we calculate the shift in probability related
to each likelihood ratio. We obtain the following results.
This means that if a sign has a likelihood ratio of
10, your patient, who has the positive sign, has 45% more chances of having the
disease. As well, if your patient has a sign whose is 0.2, he has 30% less
chances of having the disease.
If we
apply these to our example, we obtain this:
Dr. McGee proposes to simplify the results and to consider
only values above 3, which correspond to a 20% increase in probability, and
below 0.3, which correspond to a 25% decrease in probability14. In our case the results are much more simple :
Now as a clinician, if your patient has Fluid wave and
Edema, you know that he has 25% + 30% = 55% more chances of having an ascites.
On the other hand, if your patient doesn’t have Edema and has Flank tympany,
then he has 55% less chances of having Ascites.
Let’s apply this to our confusing example; remember we
had Bulging flanks (+ 15%), shifting dullness (+ 15%), fluid wave (+30) and an
absence of all the other features (- 50%). Thus, our patient has 10% more
chances of having ascites by the findings of physical examination alone.
Of course we should incorporate this in a whole process
of reasoning including the patient’s history and para-clinical features but it
is a simple and fast way to rationalize data and make the most practical use of
it in order to save time and money and help you know what is really going on in
your patient.
In fact, if you can master this, it would be as if you
personally examined all the patients in the studies and remembered how accurate
the bedside exam was for each of them!
Physical examination assessment and teaching
Teaching and evaluating physical examination skills is
a very challenging issue. Assuming that the teacher is himself qualified and skilled
enough, it is very hard for him to teach his techniques, and even harder to distinguish
among his students those who have really mastered them. Have you tried to teach
cardiac or pulmonary auscultation abnormalities to a student? It is easy to
tell him that this patient has a pneumonia and that he should hear crackles,
and he will often tell you that he had indeed listened to them, but how can you
be sure of that? And even if you are, how can you be sure he will recognize
crackles next time he hears them? Even worse are physical signs that do not obey
the dichotomous answer present/absent. How to teach your student that this deep
tendon reflex or this mitral valve S1 sound is exaggerated or diminished?
Here again we do not pretend to give solutions, but we
must point out some major mistakes present in the medical curriculum. First,
many studies show a very big lack in new generation doctors skills15, 16 and
This is due to the very little attention given by medical curriculum to
clinical examination, even in traditional programs, and this is way far from
being resolved by simple lecture courses16. The only method that seems reliable is more hours of
practice and more patient-focused training sessions. The willingness of going
in contact with patients and examine them must be taught and established in
very early stages of medical curriculum, otherwise future doctors would get
used to being away from patients and remain like that for the rest of their
careers.
Perhaps the best illustration of the commitment of a teacher
is the famous sentence of Baily, while asking his students to perform a rectal
examination: “If you don’t put your finger in, you might put your foot in it”.
Another problem of physical examination teaching is
the lack of a precise organized plan and check-list. Of course techniques and
tricks are taught everywhere, but very few textbooks provide general
examination sequences. This is due to the idea that a physician
should build his own sequence, however we believe (from experience) that most
of medical students get confused and don’t know how to start their physical
examination and whether they performed all the techniques required or not. We invite
you to take a look at this study showing most physical examination mistakes
among young physicians17.
One can easily notice that most of these techniques are well known and quite
easy to master, physicians simply forget to use them, this can be prevented
with a simple checklist.
As a result of these issues, not only did our skills
severely decrease, but also we believe that it is impossible for us to go
further! We do not even try. We all agree that old doctors know how to diagnose
a valvulopathy by auscultation alone where it is still difficult for us to
recognize a stenosis bruit... And we convince ourselves that it is not a big deal
as long as we have CT and ultrasound. In fact, we do not even know how far we
can go with physical examination. For example, where it is hard for us to
recognize dullness or tympany, Adolphe Piorry described nine distinct
percussion sounds. Holmes and the neurologists of the early 20th century used
to make diagnosis of patients before entering the examination room, simply by
hearing the rhythm and pitch of their steps as they walk! We highly invite you
to read what Conan Doyle (who was a doctor by the way) used to say about his
master, Joseph Bell, and how he could obtain a tremendous number of information
from his patients with only inspection.
Finally, one big problem in learning physical examination
is the incredible amount of new information and techniques provided in each
course, it is very difficult to remember them all. We believe that one really
effective way to help students is to include the underlying mechanisms and
pathophysiology of each sign and examination method. Students will then
understand and conclude rather than stupidly memorize and recite. As a good
example, the book “Mechanisms of clinical signs” by Dennis & al18 is really helpful for students and such initiatives
should be encouraged both for textbooks and researches.
Conclusion
Physical examination has always been and still is a
pillar absolutely necessary to medicine, and should remain so. Beyond its
scientific and pedagogic values, it is truly in its humanistic dimension that
basic bedside examination is ineffable. It is the only way to put the patient
in the center of the question and remember his need all the time. More than a
simple multitask sequence, it is an important ritual necessary for the
physician to gain patients trust and respect and to definitely seal the
patient/ physician relationship. Because patients are priceless, the “Doctor’s touch”
is obediently the proper way to bring back medicine to its original purpose: to
care about patients. As students or physicians, we should of course make the
best of new discoveries and technologies but never forget that there is a real
person behind each case, and perhaps the truth is not very far from him, as used
to say William Osler: “Listen to your patient, he is telling you the
diagnosis.”
References
1- Orient, J. M., & Sapira, J. D.
(2010). Sapiras art & science of bedside diagnosis. Philadelphia:
Wolters Kluwer Health/ Lippincott Williams & Wilkins.
2- Ranganathan, N., Saksena, F. B.,
& Sivaciyan, V. (2006). The art and science of cardiac physical
examination. Totowa, N.J: HUMANA PRESS.
3-
Simel, D. L., Rennie, D., & Keitz, S. A. (2009). The rational clinical examination: Evidence-based
clinical diagnosis. New York: McGraw-Hill.
4- McGee, S. R. (2017). Evidence-based
physical diagnosis. Philadelphia, PA: Elsevier.
5-
https://stanfordmedicine25.stanford.edu/
6- Glasziou P, Burls A, Gilbert R.
Evidence based medicine and the medical curriculum. BMJ.
2008;337:a1253.
7- Sackett DL, Rennie D. The Science of
the Art of the Clinical Examination.
JAMA. 1992;267(19):2650–2652.
8-
Crombie DL. Diagnostic process. J Coll Gen Pract. 1963;6:579-589.
9- Steve McGee M.D. Conference at
Stanford25 : https:// www.youtube.com/watch?v=0vSuPSVcWXA
10- Peter R. Orszag (2008). Increasing the
Value of Federal Spending on Health Care. Congressional
Budget Office.
11- Cattau EL, Benjamin SB, Knuff TE,
Castell DO. The accuracy of the physical examination in the
diagnosis of suspected ascites. JAMA. 1982;247:1164-1166.
12- Simel DL, Halvorsen RA, Feussner JR.
Quantitating bedside diagnosis: Clinical evaluation of
ascites. J Gen Intern
Med. 1988; 3:423-428.
13- Cummings S, Papadakis M, Melnick J,
et al. The predictive value of physical examination for
ascites. West J Med. 1985;142:633-636.
14- McGee S. Simplifying likelihood
ratios. J Gen Intern Med. 2002;17:646-649.
15- Kern DC, Parrino TA, Korst DR. The
Lasting Value of Clinical Skills. JAMA.
1985;254(1):70–76.
16-
Mangione, S., Peitzman, S.J., Gracely, E. et al. Creation and assessment of a structured review
course in physical diagnosis for medical residents. J Gen
Intern Med (1994) 9: 213
17- Wiener S, Nathanson M. Physical
Examination Frequently Observed Errors. JAMA.
1976;236(7):852–855.
18- Dennis, M., Bowen, W. T., & Cho,
L. (2016). Mechanisms of clinical signs. Chatswood, N.S.W.: Elsevie







Commentaires
Enregistrer un commentaire