When Cancer Catches the Flu
When Cancer Catches the Flu
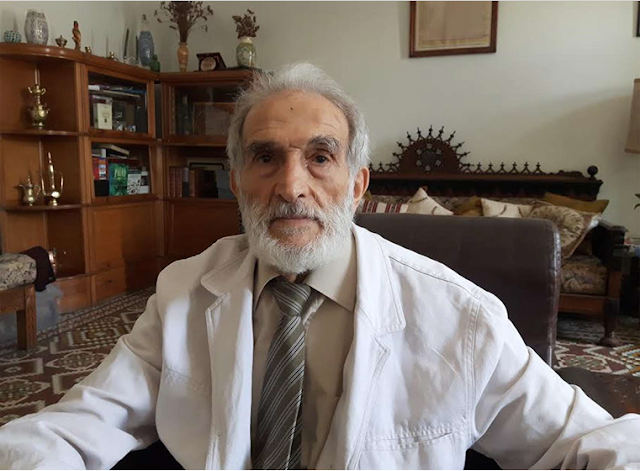
Rihab FELLAH
Historically, cancer was thought to be caused by viruses, though this remains true for some types. Today we are using those same agents to fight cancer. Indeed, virotherapy is at the forefront of the latest advancements in Microbiology, Immunology and Molecular Biology and offers interesting prospects in the field of oncology.
Virus have always been known to be remarkable microbes. From the Influenza Virus to the HIV, they have ability to replicate inside cells by exploiting cellular resources. They can cause at the end of their reproductive cycle a lysis of the host cell, which makes them one of nature’s most effective killers. Science, however, has found a way to exploit this skill in a more efficient way: killing cancer cells. Making, therefore, oncolytic viruses (OVs) the latest leap in oncology and its armamentarium. This encounter goes back to the early to mid-20th century. When regressions of tumoral growth have been observed in cancer patients suffering from viral infections. Though these regressions were temporary and rarely complete, they couldn’t but spark some hope that a novel cancer therapy has been discovered. The pursuit of such thought was halted due to the little understanding researchers had at the time of carcinogenesis and microbiology. Also, the great success that had been demonstrated by chemotherapy and radiotherapy in treating cancer prevented it too. Today, in the era of genetic engineering and recombinant DNA technology, viruses can be manipulated to be less harmful towards healthy cells and to infect tumoral ones in a specific way. They offer a more targeted way of treating cancer than that found in chemo and radiotherapy, with minimal side effects. In 2015, researchers were at the cutting edge of cancer therapy when T-VEC–a genetically modified HSV type 1– became the first oncolytic virus to be approved by the FDA (Food and Drug Administration) and the EMA (European Medical Agency) for the treatment of unresectable melanoma.
How do oncolytic viruses work exactly? They have many mechanisms of action. For starters, OVs whether natural or genetically engineered and/or modified are, by definition,
viruses that have a particular tropism to cancer cells. They are incapable of replicating elsewhere. In fact, many OVs are modified to express membrane proteins/receptors that interact with counterparts found only in tumoral cells. Not forgetting that these cells express little self-antigens such as HLA-1 and do not secrete IFN type I , II or TNF ( key cytokines for antiviral immunity) when infected. The lack of effective cornerstones such as these makes the antiviral immune response deficient in cancer cells, which explains their susceptibility to viral infections. It has been known that cancer cells, escape the immune system via the expression of certain inhibitory immune check points such as PD1 (Programmed Death 1) and CTLA4 (Cytotoxic T Lymphocyte Associated-protein 4). These molecules are what makes cancer cells tolerated by the immune system. Many monoclonal antibodies targeting them have been developed and approved as cancer therapies for tumors such as melanoma and offer, thus, the possibility of a combined therapy with OVs. Viruses can also be engineered to produce growth factors that stimulate antitumoral immunity. It is the case with T-VEC which expresses GM CSF (Granulocyte Macrophage Colony Stimulating Factor). OVs can also be made to activate intracellular pathways that induce apoptosis or deactivate those responsible for carcinogenesis. This is observed in Onyx 015, an engineered adenovirus that has the ability to activate the tumor suppressor p53 and therefore cause oncolysis. Though this particular virus has not been approved by the US and EU agencies due to lack of efficacy; a Chinese analog, H101, has been approved as an adjuvant to chemotherapy in the treatment of head and neck tumors in China.
The New Castle disease virus; a fowl infecting microbe and non-pathogenic to humans; can bind to human cells via HN (Hemagglutinin and Neuraminidase). It can activate Caspases (Cysteine Aspartic acid- Specific ProteASES) in cancer cells. These molecules not only work as initiators and executioners of cell death, but also have the ability to cleave Livin. A member of the Inhibitor of Apoptosis Protein (IAP) family. Livin is associated with poor prognosis when highly expressed in melanoma. Once cleaved, Livin becomes paradoxically proapoptotic, enhancing furthermore the cellular death effect of this OV. It is uncontestable that oncolytic viruses have proved their usefulness. Nevertheless, they still have their limits. First, their testing in animal models can sometimes wrongly predict the outcomes of clinical trials. Indeed, viruses are either tested in xenografts (human tumor tissue grafted in an animal) implanted in an immunocompromised mouse. Or an immunocompetent one in which a tumor has been induced in its own tissue. Both cases may not foresee the results found in clinical trials on human subjects. Another limitation, is that they still induce both an innate and an adaptive immune response. Through the former, it has been observed that OVs administered intravenously can bind to platelets and are later cleared in the liver by Kupffer cells. Through the latter, many humans are already immunized to viruses (50–80% possess neutralizing antibodies against HSV and almost 90% against Reovirus). This makes their administration exclusively intratumoral, intraperitoneal or intrapleural.
The intensive research done in this field and the little progress encountered (only two viruses approved for treatment) makes it clear that oncolytic viruses aren’t very effective as an isolated treatment for cancer. They can work in synergy with others lines of treatment. Many clinical trials are investigating these combinations. For instance, infecting immune host cells with an OV ex vivo, then injecting it back to the patient can help detour the antiviral immune defenses and deliver the virus safely to the tumor bed. This is referred to as the “Trojan horse” strategy. The difficulty lies in finding the ideal cell carrier for the patient and the tumor. Further research is being done in this regard. Another combination that has potential, is a viral bacterial combined therapy. In such a combination, the virus infects an intracellular and anaerobic bacteria. This bacteria would have enhanced chemotaxis towards tumors and would be lured by their hypoxemic regions that result from an undeveloped vascularization. Once inside, the virus would be delivered safely and can infect the totality of the tumoral tissue.
These are one of the alluring prospects virotherapy offers in the fight against cancer, humanity’s immortal enemy. The success of T-VEC with melanoma seems to be a promising start to many other achievements. Especially, that this particular cancer is one of the most aggressive ones. T-VEC has opened a door to many possibilities: involving this same agent in a combination with immunotherapy (anti PD1 and anti CTLA-4 therapy) is currently being tested. More has yet to come.
Références
- Gougis P, Teixeira L. Oncolytic Viruses: First Validation of a Therapeutic Category that is not so new. Oncologie (2016) 18:517-522.
- Fountzilas C, Patel S, Mahalingam D. Review: Oncolytic virotherapy, updates and future directions. Oncotarget, 2017, Vol. 8, (No. 60): 102617-102639.
- Wei D, Xu J, Liu X, Chen Z, Bian H. Fighting Cancer with Viruses: Oncolytic Virus Therapy in China. Human Gene Therapy. 2017.
- Bell J, McFadden G. Viruses for Tumor Therapy. Cell Host & Microbe. 2014;15(3):260-265.
- Krzykawski M. Combined bacterial and viral treatment: a novel anticancer strategy. Central European Journal of Immunology. 2015; 3:366-372.
- Tortora GJ, Funke BR, Case CL. Microbiology: an introduction ,11th ed. 2013.
- Kierszenbaum A, Tres L. Histology and cell biology. 4th ed. 2016.
- Abd-Elrahman I, Hershko K, Neuman T, Nachmias B, Perlman R, Ben-Yehuda D. The Inhibitor of Apoptosis Protein Livin (ML-IAP) Plays a Dual Role in Tumorigenicity. Cancer Research. 2009;69(13):5475-5480.
- Lazar I, Yaacov B, Shiloach T, Eliahoo E, Kadouri L, Lotem M et al. The Oncolytic Activity of Newcastle Disease Virus NDV-HUJ on Chemoresistant Primary Melanoma Cells Is Dependent on the Proapoptotic Activity of the Inhibitor of Apoptosis Protein Livin. J Virol. 2010; 84(1):639-46.
- Dine J, Gordon R, Shames Y, Kasler M, Barton-Burke M. Immune checkpoint inhibitors: An innovation in immunotherapy for the treatment and management of patients with cancer. Asia-Pacific Journal of Oncology Nursing. 2017;4(2):127.
Images: http://mariafresa.net/data_gallery/photo-cold-cough-flu-in-babies-babycenter-images-CbgX8a-clipart.jpg. Image de l’arrière plan par : Harryarts / Freepik Starline / Freepik


Commentaires
Enregistrer un commentaire